JAMA Intern Med. Published online May 23, 2016.
CChronic stress can make us worn-out, anxious, depressed—in fact, it can change the architecture of the brain.
New research at The Rockefeller University shows that when mice experience prolonged stress, structural changes occur within a little-studied region of their amygdala, a part of the brain that regulates basic emotions, such as fear and anxiety. These changes are linked to behaviors associated with anxiety and depressive disorders
There is good news, too: an experimental new drug might prevent these changes.
“There have been hints that the amygdala displays a complex response to stress,” says lead author Carla Nasca, a postdoc in Bruce S. McEwen’s lab. “When we took a closer look at three regions within it, we found that neurons within one, the medial amygdala, retract as a result of chronic stress.
“While this rewiring can contribute to disorders such as anxiety and depression, our experiments with mice showed that the neurological and behavioral effects of stress can be prevented with treatment by a promising potential antidepressant that acts rapidly,” Nasca says.
In the research, published in Molecular Psychiatry, her team found this protective approach increased resilience among mice most at risk for developing anxiety or depression-like behaviors.
A close look at the amygdala
The brain’s limbic system controls emotions and memory, and it comprises a number of structures, including the amygdala, which is found deep in the brain. Scientists interested in the neurological effects of stress have focused on several structures in the limbic system, but the medial amygdala has thus far received little attention in stress studies.
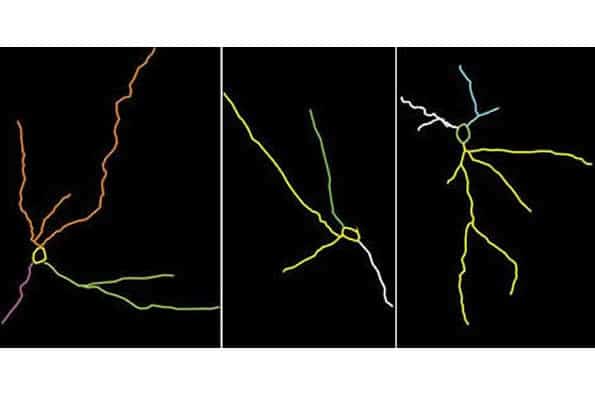
To see what was going on in this area, as well as two other parts of the amygdala, Nasca and her team first subjected mice to 21 days of periodic confinement within a small space–an unpleasant experience for mice. Afterward, they tested the mice to see if their behaviors had changed–for instance, if they had begun to avoid social interaction and showed other signs of depression. They also analyzed the neurons of these mice within the three regions of the amygdala.
One area saw no change with stress. In another, the basolateral amygdala, they saw that neurons’ branches became longer and more complex—a healthy sign of flexibility and adaptation, and something that had been shown up in previous work. But in the medial amygdala, they neuronal branches, which form crucial connections to other parts of the brain, appeared to shrink. The loss of connections like these can harm the brain, distorting its ability to adapt to new experiences, leaving it trapped in a state of anxiety or depression.
Protecting neurons
This effect could be prevented. The scientists repeated the stress experiment, and this time they treated mice nearing the end of their 21 days of chronic stress with acetyl carnitine, a molecule Nasca is studying for its potential as a rapid-acting antidepressant. These mice fared better than their untreated counterparts; not only were they more sociable, the neurons of their medial amygdalas also showed more branching.
Stress does not affect everyone the same way. This is true for both humans and mice—some individuals are just more vulnerable. Nasca and her colleagues’ experiments included mice at high risk of developing anxiety- and depression-like behaviors in response to stress. Treatment with acetyl carnitine also appeared to protect these mice, suggesting that a similar preventative approach might work for depression-prone people.
Both humans and rodents naturally produce acetyl carnitine under normal conditions and several depression-prone animal models are deficient in acetyl carnitine. In a separate study, Nasca and colleagues are examining whether people with depression have abnormally low levels of the molecule.
“Chronic stress is linked to a number of psychiatric conditions, and this research may offer some new insights on their pathology,” McEwen says. “It seems possible that the contrasting responses we see within the amygdala, and the limbic system in general, may contribute to these disorders’ differing symptoms, which can range from avoiding social contact to experiencing vivid flashbacks.”
Note: Material may have been edited for length and content. For further information, please contact the cited source.
Publication
Lau T et al. Stress-induced structural plasticity of medial amygdala stellate neurons and rapid prevention by a candidate antidepressant. Molecular Psychiatry, Published May 31 2016. doi: 10.1038/mp.2016.68
© Business Name. All Rights Reserved.